By Terri Somers
Senior Manager, Global PR and StoryLab
 Scott Meech and his wife, Samantha, hiking in Spain earlier this year.
Scott Meech and his wife, Samantha, hiking in Spain earlier this year.
“The disease, nowadays, is considered more of a chronic condition because we have been putting patients into better treatment plans that produce excellent outcomes, elongate their remissions and allow for a better quality of life,” he said.
“For instance, researchers have found that adding a new immunotherapy drug to the first line of treatment reduces the chances of a patient getting worse or dying by about 40% to 60%, while also lengthening remission by roughly 15% to 20% after 4 to 5 years,” he said.
Scott is an example of that evolution.
With an elevated risk of myeloma given his sister’s illness, Scott was monitored with blood tests for almost two decades. One of those tests, called Freelite®, was launched in 2001 by the Binding Site, a company acquired in 2023 by Thermo Fisher. In 2018, abnormal test results prompted Scott’s doctor to investigate further, confirming he had developed myeloma. The result, he said, is a cancer journey drastically different than his sister’s.
“I can honestly say that I've never felt any of the symptoms of myeloma,” Scott said. “That is a stark contrast to my sister’s experience having the damaging symptoms of advanced disease.”
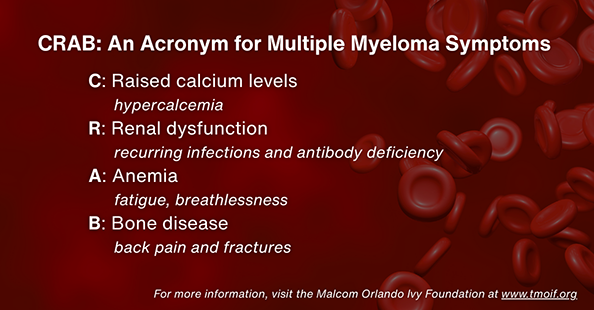
To understand the magnitude of that improved outcome, one must comprehend the complexity and challenges of myeloma. It is an incurable and heterogeneous disease. There is no typical journey and no one-size-fits-all treatment.
Myeloma is an elastic and persistent cancer, Luis said. Diagnosis usually occurs after the cancer has damaged organs and formed multiple lesions, or myelomas, in the patient’s bones—hence the name of the disease. Once treatment begins, patients experience a journey of peaks and valleys, periods of increased cancer activity that may be quieted, followed by relapses and additional rounds of treatment. Often, myeloma becomes resistant to one therapy, challenging doctors to find a subsequent treatment that will work. On average, a myeloma patient receives five different treatment protocols, Luis said.
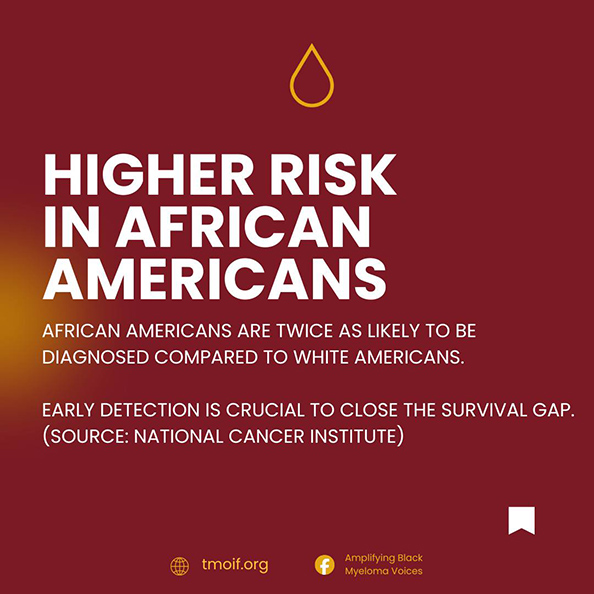
Research suggests that both genetics and environmental factors may play a role in the development of myeloma, though there is no known inherited genetic mutation that is the driver of the disease, as there is in other cancers, such as breast, prostate and lung cancers, said Stephen “Ste” Harding, vice president and general manager of the Protein Diagnostics business within Thermo Fisher. There is also no recommended testing for myeloma at a certain age, as there is for some other cancers. However, ongoing studies aim to determine whether recommended testing at a specific age could contribute to earlier diagnosis and potentially improve outcomes, said Ste, one of the researchers involved in one such study.
Scott said that, in retrospect, he believes he was fortunate to know he was at risk of myeloma because his compliance with quarterly blood monitoring enabled an early diagnosis and improved his journey.
Comparatively, patients who do not know they may be at risk of developing the disease might spend months seeing medical specialists before they are finally diagnosed, Luis said.
 Scott Meech enjoying his photography hobby in his garden.
Scott Meech enjoying his photography hobby in his garden.
For Scott, the presence of MGUS, coupled with a first-degree family connection to myeloma, meant he had an elevated risk. Doctors explained that blood tests every few months would allow them to monitor Scott for signs that MGUS was evolving into myeloma. One of those tests would monitor the accumulation of M proteins. The second, Thermo Fisher’s Freelite, monitors the accumulation of another indicator protein, free light chains, produced by rogue plasma cells. Studies have shown that these tests together can diagnose 99% of myeloma cases, Ste said.
“It was pretty terrifying for a while,” Scott said of learning he had an elevated risk. “My wife and I were in our early 30s and had two young children. It framed a lot of our lifestyle choices.”
 Scott Meech and his daughter, Lily, after she finished the 2025 London Triathlon in just over 3 hours.
Scott Meech and his daughter, Lily, after she finished the 2025 London Triathlon in just over 3 hours.
 The EXENT System
The EXENT System
The EXENT System uses mass spectrometry to detect myeloma-related proteins based on their mass and can identify them at very low concentrations in the patient’s serum. The monitoring support* function approved in Europe is key for asymptomatic myeloma patients because it may allow them to avoid a number of excruciating bone marrow biopsies, said Ste, the vice president Thermo Fisher’s Protein Diagnostics business.
“No one wants three or four bone marrow biopsies a year,” he said. This improvement in patient care, Ste said, exemplifies the myeloma expertise that Thermo Fisher has amassed over more than two decades. “We’ve only ever wanted to improve the outcomes of patients from multiple myeloma.”
The EXENT System has earned regulatory clearance as an aid in the diagnosis and monitoring of multiple myeloma in Europe, Brazil and Australia. It is authorized for sale by Health Canada and is commercially available in New Zealand.
In the United States, it is cleared for use to aid in the diagnosis of multiple myeloma.**
“The biopsy process is something that myeloma patients dread,” Scott said, “In the UK, the biopsy is done with a locally injected anesthetic. The injections numb the flesh but not the bone itself, so when the bone is penetrated, it can be pretty painful.”
There’s also a psychological benefit for the patient in having access to such sensitive testing, Scott said. In previous tests, when his protein levels increased by one point, Scott’s clinicians would tell him not to worry too much, since it could be a test variable or a reading error.
“But I do worry about it,” Scott said. “So having that specificity (of EXENT) is extraordinary. The more knowledge I have as a patient, and I’m sure I speak for a lot of patients, it gives us more confidence and more optimism that the right thing is being done.”
Thermo Fisher has been a part of myeloma research and discovery for decades, Luis said. During that time, it has amassed research data and expertise that enable its customers at all stages of drug development, he said. Its knowledge and technology also empower clinical trials that encompass broad patient representation, including those from high-risk populations and people in geographic areas that may otherwise lack access to the latest drugs and diagnostics, he said.
Meanwhile, customers have used Thermo Fisher’s next-generation sequencing (NGS) products for both companion diagnostics and research-based studies.
In addition, researchers developing new therapies can use NGS tools to peer deeply into the DNA of malignant plasma cells, providing more information about what’s driving myeloma, said Luisa Campos, from the medical education and grant office of Thermo Fisher’s NGS business. This information can reveal insights that help better understand why some patients respond to therapies and others don’t. And it may be used to identify novel genetic mutations that could serve as targets for future treatments, she said.
Scott is comforted by innovations in research and technology, and by the quest to develop new therapies and diagnostics that may help him and fellow myeloma patients enjoy many years ahead. Meanwhile, 1 million of his stem cells are in a freezer as a future treatment option, along with several other therapies developed in recent years that have shown tremendous effectiveness for myeloma.
“It seems to me,” he said, “that we’re in a bit of a golden age of advancement in all sorts of medicine and diagnostics.”
*The following information relates to uses of the EXENT Immunoglobulin Isotypes (GAM) for the EXENT Analyser test system that are authorized in certain markets outside the United States. Availability, indications, and regulatory status vary by country. The EXENT Immunoglobulin Isotypes (GAM) for the EXENT Analyser test system has not been evaluated for use in post-diagnostic patient monitoring of monoclonal gammopathies, in the USA.
This information is intended for healthcare professionals in regions where these uses are authorized.
**For full product information, please consult the product labelling.
U.S market information only: Rx only. Serum matrix only. Results require valid Optilite® IgG/IgA/IgM results on the Optilite Analyzer. For use as a reflex test when serum protein electrophoresis suggests an M‑protein or when serum free light chains are abnormal
EXENT, Optilite and Freelite are trademarks of The Binding Site Group Ltd (Birmingham, UK) in certain countries.